Date:16 March 2023
Content Sections
- ● It’s Bigger Than Me movement
- ● Conflicts of interest
- ● Lack of will power, poor lifestyle choices or disease?
- ● Changing the record
- ● A blockbuster market
- ● Jumping on the bandwagon
- ● Hidden harms
- ● Taking back control
By Melissa Smith, outreach and communications officer, ANH Intl, and Rob Verkerk PhD, founder, executive & scientific director, ANH Intl
There’s a new kid on the weight loss block. One that’s guaranteeing significant weight loss from just one teensy injection a week. It comes with the promise that it’s a powerful tool to end the obesity epidemic. Not only that, now that the world is so accustomed to jabs, the public is being told that with Novo Nordisk’s latest offering, wegovy® (semaglutide), you won’t even have to change your diet or lifestyle to lose those pounds.
That’s a very big ask given Big Pharma’s chequered history with anti-obesity drugs. There have been a succession of failures, nominal benefits, a cascade of side effects, eye-watering pricing, including even one (lorcaserin) that increased cancer rates before being pulled from the market by the US Food and Drug Administration.
Despite this motley background, Big Pharma is far from giving up. With obesity rates continuing to spiral, the market it just too big and potentially lucrative to not give it a go.
To help us be less questioning over the possibility of another failure, Novo Nordisk is keen to change the conversation around obesity.
You know when someone tries to change the conversation to stop you asking questions about things they don’t want to talk about? Well, that’s what this is about.
It’s Bigger Than Me movement
Spearheading its approach is Novo Nordisk’s establishment of – wait for it – a ‘movement’. The new movement is called It’s Bigger Than Me – and Queen Latifah is among Novo Nordisk’s paid spokespersons. Knowing just how keen Novo Nordisk is to get people to line up for its weekly jabs if their BMI exceeds 35, there’s something deeply unsettling about it. That’s got something to do with the fact we know properly informed consent that gives people a choice of options won’t be practiced, there’s a lack of data on long-term effects, and it’s now open sesame given regulators around the world have green lighted the new drug.
Predictions by the World Obesity Atlas 2023 suggest that over half the global population will be overweight or obese by 2035. Yes, that’s enough to get any board room contemplating routes to market for its latest anti-obesity offering excited.
As with so many previous offerings presented by Big Pharma as magic bullets, there’s often a sting to be found hiding away around the rear end of the beast.
Let’s go hunting…
Conflicts of interest
Novo’s ‘skinny’ jab built around the GLP-1 (appetite suppressant) analogue semaglutide, goes under one of two brand names, Wegovy or Ozempic. The jab has received plaudits from across the world (here and here) in order to sell a ‘fix’ for the obesity epidemic. The support given by key health professionals has seen the UK’s NHS make Wegovy available via pharmacies without prescription. It’s also become the go to for celebrities looking to drop a few pounds quickly.
Yet the buzz driving this new ‘miracle’ obesity treatment comes not only from Novo’s new movement, but a concerted campaign laden with conflicts of interest funded by Novo Nordisk to the tune of £21.7m. This money has been paid to health organisations and professionals across the healthcare spectrum to promote the drug, most of whom have concealed or been reticent in revealing their association.
Even World Obesity Day, which takes place on the 4th March each year, isn’t free from industry influence. This year’s theme was ‘Changing perspectives. Let’s talk about obesity’. An interesting title given the sudden push for the use of obesity drugs. Or perhaps not – especially when we find out that World Obesity is funded by the very organisations set to profit from obesity drugs.
The American Academy of Pediatrics is staying loyal to its paymasters by publishing updated guidelines stating obesity is a disease that needs to be treated early and aggressively. Its recommendations include the use of obesity drugs for children.
Lack of will power, poor lifestyle choices or disease?
Obesity, which has traditionally been viewed as a lifestyle issue, often blamed on a lack of will power, is now being framed as a chronic genetically-associated disease that demands treatment with appetite suppressant drugs like semaglutide (Wegovy or Ozempic), tirzepatide (Mounjaro) or a mix of semaglutide and cagrilintide, an amylin analogue, branded as CagriSema.
The ‘new’ obesity drugs are part of a class of drugs called incretin mimetics or GLP-1 based drugs, which imitate the effects of a hormone called glucagon-like peptide 1 (GLP-1) that can make people feel full, so suppressing appetite. Until now, they’ve been one of the pharmacological treatments used for type 2 diabetes. While they can cause a large amount of weight loss, up to a fifth of body mass, they tend to have to be taken regularly by injection to avoid piling the pounds back on.
These drugs work by curbing appetite and slowing digestion so less food is consumed. However, obesity is a complex multi-factorial condition that decades of clinical experience has shown requires a multi-factorial approach to resolve it. The GLP-1 based drugs only target one part of our appetite control system, ignoring the role of hormones such as leptin, ghrelin, glucagon and a bunch of neurotransmitters. This means the drugs don’t tackle the root cause of the issue and provide only a quick fix that works only as long as you depend on the drugs.
All this before you even start considering the roles of addiction and reward circuitry, chronic and oxidative stress, and social pressure to conform to societal behavioural and dietary ‘norms’, better thought of as ‘abnorms’, created to maintain the imbalance of both weight and power.
Good for Novo Nordisk’s and Eli Lilly’s business, not so good for us.
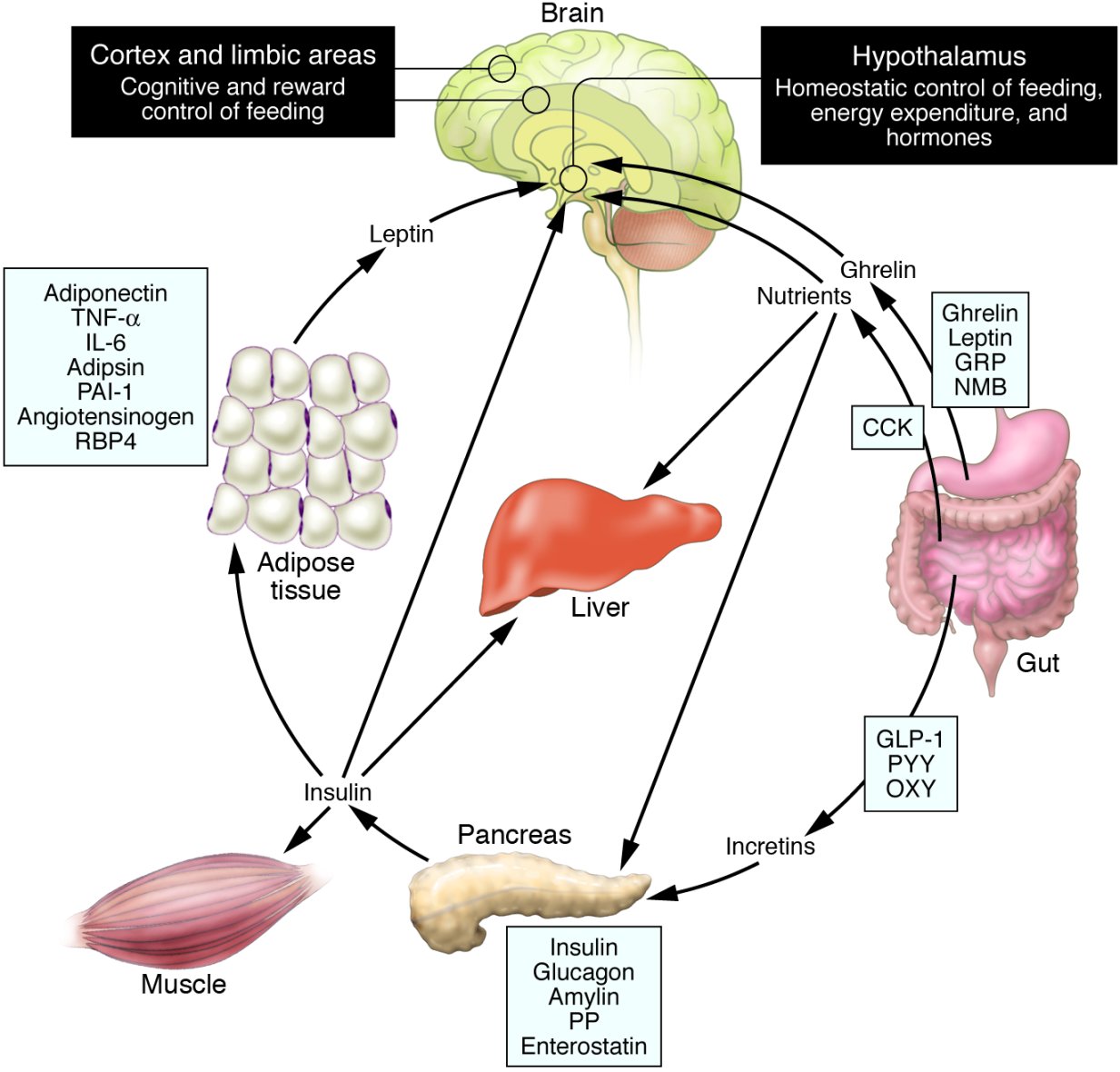
Schematic illustration of peptides secreted by the gut and adipose tissue (fat) that control energy balance.
Source: Ahima RS. J Clin. Invest. 2008; 118(7): 2380-2383.
Changing the record
The push behind Novo’s ‘skinny’ jabs contradicts previous corporate attempts to normalise our attitudes towards being fat. For a while, we have been sold the idea that we can be fat and healthy, an idea which ignores a plethora of research that points to the increased risks of developing cancer, heart disease and type 2 diabetes along with a wide range of other serious health conditions that accompany obesity.
In recent decades doctors have become increasingly hesitant to tackle obesity due to the body positivity movement, which has its roots in the 1960s, known back then as the Fat Acceptance Movement. More recently it has become a marketing tool that seeks to promote inclusivity.
Published science is taking things one step further to reassure us that being fat can be healthy. A Danish study published in JAMA, spanning almost four decades and involving more than 100,000 adults found that those with an ‘overweight’ body mass index (or BMI) were more likely to live longer than those in the ‘healthy’, ‘underweight’, and ‘obese’ categories.
Even Daily Mail columnist, Amanda Platell, has had an epiphany leading her to eschew her decades-long fat shaming ways and declare that fat can be fabulous.
Despite the push to normalise being overweight and obese, the cost and impact of obesity and its associated conditions is hitting home as healthcare systems start to buckle under the pressure and quick fixes are sought to stop the tsunami.
A blockbuster market
The huge profits to be made from obesity drugs is manna to the pharma. The obesity drug market is predicted to increase over 6% by 2027 and the global obesity market is projected to be worth around $50 billion by 2030.
A recent report estimates the economic cost of obesity in the UK alone tips the scales at £58 billion. That might sound shocking until you realise that the report has been commissioned by none other than the beneficiary of the new conversation around obesity, Novo Nordisk.
In the US, the economic consequences of obesity are estimated to be an eyewatering $125 billion annually.
The size of this market is as such that other pharma companies are now racing to cash in, including Pfizer, which is currently developing its own obesity drug.

Jumping on the bandwagon
Even WeightWatchers has announced it is moving into telehealth so it can tap into the lucrative world of obesity drugs. Another moving conversation, one that takes the weight loss giant away from its traditional market of weight loss clubs and calorie counting, straight into the unfolding paradigm of sit-on-the-couch and get-yourself-jabbed.
Nestlé Health is hyping an ingestible that delivers a bag that inflates in the stomach, then allegedly breaks down within the digestive system after a few hours. Despite the hype, the product hasn’t yet entered clinical trials.
Scientists are also working on deep brain stimulation. This uses an implanted device that electrically stimulates a key area of the brain (nucleus accumbnens) that controls binge eating.
Hidden harms
The stampede to launch a new generation of drugs to tackle obesity has caused concern among some critics, who are warning about their potential for misuse and serious side effects. The drugs come with a raft of serious adverse reactions such as nausea, vomiting, diarrhoea, acute kidney injury along with an increased risk of developing thyroid cancer. Chinese scientists publishing in Acta Pharmaceutica Sinica B warn that weight loss drugs such as Wegovy could result in blockages in the small intestine.
If you’re lucky enough to overcome the adverse reactions, then there’s the significant problem that as soon as you stop taking the drugs, the weight piles back on as many are already finding out (here and here).
Taking back control
You’ll find below a variety of articles, videos and resources below to help you understand the complexity of our body’s metabolism, and take back control of your health journey to reach optimum wellbeing and vitality through regaining metabolic flexibility.
>>> RESET EATING is our book about it – and it’s now available on Kindle as an ebook.
>>> ANH-Intl Feature: Are governments deliberately on the wrong anti-obesity track?
>>> It’s the type of fuel, not the quantity that really matters
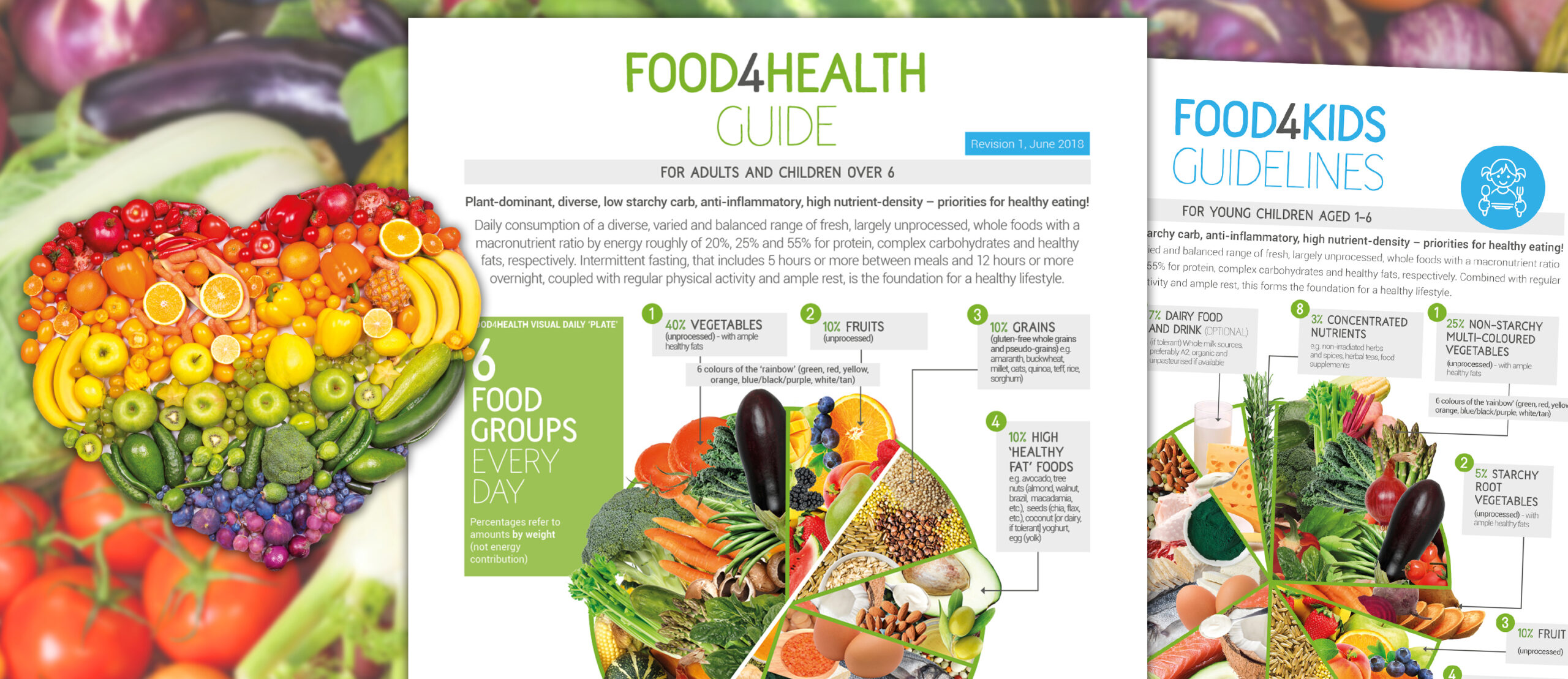
>>> ANH Food4Health guidelines
>>> Buy a copy of RESET EATING to help you reset your health and resilience
>>> Reversing diabetes naturally: The evidence
>>> Calling time on eating little and often
>>> Fat – probably the least understood endocrine organ
>>> Top 10 causes of adult obesity
>>> Obesity: the deadly dance between immunity and metabolism
>>> Is taxing our way out of obesity the answer?