Date:22 February 2024
Content Sections
- ● Neuroendocrinology
- ● Menopause metabolism
- ● Solutions! What to do to minimise ‘menopause brain’
By Meleni Aldridge, executive coordinator
Are you a woman of a certain age experiencing brain changes and pondering this valid question – is ‘menopause brain’ really a thing? Or do have you a loved one that you think fits this bill?
Given these days how many women—particularly those who’re in, or are approaching, menopause—are talking openly on social media and elsewhere about signs of hormonal imbalance and dysfunction, you could be of the view that nature has created a life stage that disadvantages women. Or that menopause, and its symptoms, requires treatment and should be medicalised.
Or perhaps we’re outliving our invitation to be here, living longer than nature intended once our child-bearing usefulness is over? Or maybe the chasm between our genetic blueprint, evolutionary history and modern life is widening and taking its toll on women’s health?
At ANH, our view is that menopause is an entirely normal stage in a woman’s life. We simply don’t subscribe to the view of many drug regulatory authorities which, undoubtedly prompted by their revolving doors with Big Pharma, are trying to medicalise the life stage. No, we submit that menopause is a key life stage that every woman, who still has her ovaries, will reach in her life if she lives past her fifties. But when viewed through the lens of conventional medicine, it’s a life stage that isn’t well understood, mainly because it’s only recently that there’s been acknowledgement that there are many more differences between men and women’s bodies that go way beyond anatomy. Most of the early clinical research that built the foundations of modern medicine as we know it was conducted on men and much of the ongoing research still is. Not only that, If women want to manage menopausal symptoms, hey, why not just prescribe synthetic hormone replacement therapy (HRT) and ignore the fact this will likely increase the risk of breast cancer and endometrial hyperplasia (a thickening of the uterine lining)?
Neuroendocrinology
In the human body, nerves (neurology) and hormones (endocrinology) are two communication systems that work hand in hand. Your neurological system is like a super conductive highway throughout your body that enervates every thought, action and reaction. Hormones are messenger molecules that direct and govern your biological actions.
In a woman’s body, our neurology and our hormones work in tandem, far more so than in a man’s body where the prime hormone mover is testosterone that pulses in 15-20 min bursts during a 24-hr period throughout life.

“Brains and ovaries are part of the neuroendocrine system. The brains talk to the ovaries and the ovaries talk back to the brain.” – Lisa Mosconi PhD.
We women on the other hand, have a suite of hormones that need to work in synergistic flow, as well as with our neurology, immune system and metabolism. You may not be aware that oestrogen is also involved in a woman’s brain function, with oestradiol specifically being critical for energy production in the brain. This is why a woman can lose around 30% of brain energy after menopause. Please note I’ve said brain energy, not brain function. There is a difference.
Contrary to conventional thinking, new research carried out by Lisa Mosconi PhD and her team in the Women’s Brain Initiative at Weill Cornell Medicine, clarifies that menopause symptoms like hot flushes (or flashes if you’re American), brain fog and memory loss are not hormonal, but neurological symptoms caused by low brain energy in specific areas. The effects being more potent in certain areas of the brain. In the case of hot flushes/flashes it’s the hypothalamus not regulating temperature correctly, an underpowered frontal cortex causing brain fog and ebbing oestrogen in the amygdala responsible for the increased ‘senior moments’. When our oestrogen is high, so too is our brain energy.
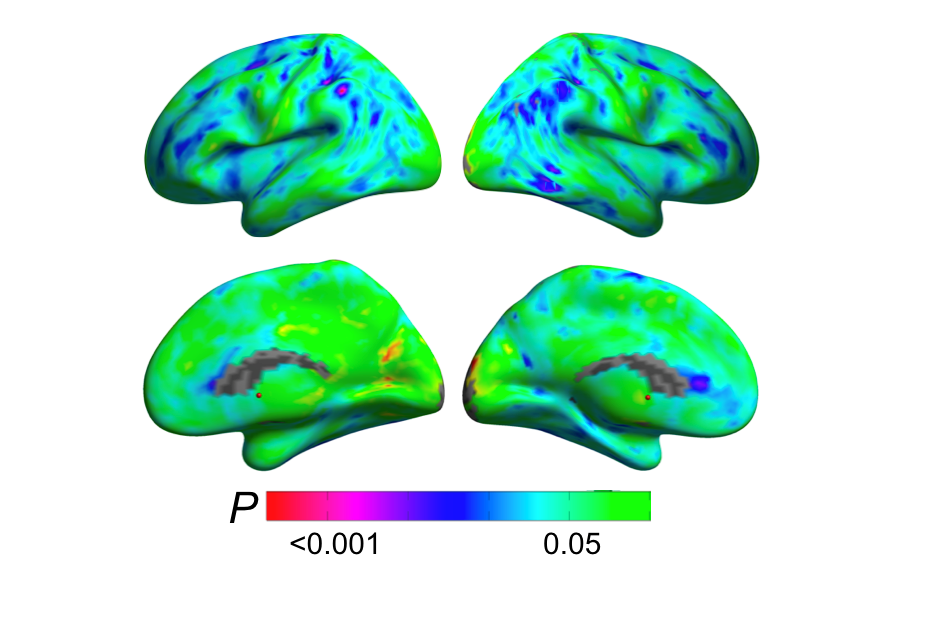 Source: Imaging Study Reveals Brain Changes During the Transition to Menopause. Women’s Brain Initiative, Weill Cornell Medicine, Lisa Mosconi PhD.
Source: Imaging Study Reveals Brain Changes During the Transition to Menopause. Women’s Brain Initiative, Weill Cornell Medicine, Lisa Mosconi PhD.
Correspondingly, when our oestrogen is low, our brain energy drops, which long-term as in menopause, can cause our neurons to age faster. This is the reason why women have a two-fold risk to men for developing dementia, because low brain energy sets up a milieu in which amyloid plaques can develop. Whilst amyloid plaques are not the cause of dementia, they create increased risk, especially in the presence of insulin resistance, metabolic dysfunction and low-grade, chronic inflammation.
You’ll recognise the same bad actors responsible for creating the environment in which chronic diseases flourish. Dr Mark Hyman, in his interview in the recent Better Brain Blueprint documentary series, confirmed that you can have a brain full of amyloid plaques with no evidence of dementia, but it’s the combination of plaques and inflammation from metabolic dysfunction that tips a brain over the edge.
The ebb and flow of oestrogen is a natural part of a woman’s menstrual cycle and understanding the neurological connection explains so much about our complexity. We really do experience changes in mood and cognitive function during the month related to our hormonal flow. In mid-life our brains can become even more sensitive to our hormones in the lead up to menopause, which is why peri-menopause (the period before actual menopause begins) brings with it so much change.
I hope there are some big aha moments happening as you read this. You’re not crazy, you just need to understand the power and impact of your hormones and work with them, not against them.
If you have a menstrual cycle, it’s so important to track and understand it because you can then live your life in flow and make the most of your high energy time, which is also your most creative time and the best for problem-solving. In her interview with Jim Kwik, Dr Mindy Pelz goes as far as saying that businesses should put all their ovulating women in a boardroom and say, “OK, let’s dream up what next year’s going to look like”! She may be joking, but you get the picture. Hormones really matter for women’s brains.
Menopause metabolism
We’ve looked at menopause as a dynamic neurological transition that significantly impacts brain structure and connectivity, but it’s essential to understand its metabolic impacts too. Here again we see the impact of oestrogen as it’s not just the brain that suffers from its loss. As oestrogen nosedives during menopause, we become more insulin resistant, which impacts our body’s energy uptake.
Insulin resistance results when our tissues (e.g. adipose [fat], skeletal muscle and liver), no longer respond appropriately to insulin, causing the ineffective uptake of glucose into the cells, leaving it circulating in the blood. The more insulin resistant we become, the more increased the risk for developing type 2 diabetes, along with abdominal obesity (hello ‘menopause tyre’…), high blood pressure and dysregulated fat handling — all components of metabolic syndrome, which in turn, significantly increases the risk of developing cardiometabolic (heart-related) disorders.
Sounds like it’s all fun, fun, fun, doesn’t it? Don’t despair, we’re about to get on to what to do about it. Nature really hasn’t messed up and deep in our genetic blueprints are the safeguards for both our brains and our bodies during menopause and beyond.
Solutions! What to do to minimise ‘menopause brain’
Our genetic blueprint holds the key to transitioning to the new post-menopause normal, but the route in, like for all health creation actions, is through the metabolism—the energy creation pathways that power life. Employing most, if not all, of the following suggestions will not only give your brain the maximum support through this very normal, physiological life-stage, but also put you onto the most beneficial health and longevity trajectory.
- Transition to a low (not zero) carb lifestyle. Cut out all refined, processed and ultra-processed carbs in the form of cakes, biscuits, pasta, sweets, candies and milk chocolate. Limit grains (omit gluten-containing grains) from your daily nutrition and instead increase your above-ground plant foods (chard, kale, spinach and all the cruciferous veg like broccoli, cabbage and cauliflower). Nature intended us to eat sufficient quantities of complex carbs from plants, which also give us the all-important fibres we need to create and maintain a healthy microbiome. Use root vegetables (e.g. carrots, parsnips, beets, sweet potatoes) and squashes (e.g. pumpkin, butternut, gourds) to offer additional natural sugars. Choose low glycaemic fruits like less sweet apples (e.g. Granny Smiths), pears and berries and have them after a meal, not on their own, in moderation.
Peri-menopausal and menopausal women need more carbs than a traditional keto diet allows, as we need to support hormone production. It’s a delicate balance as insulin is needed for oestrogen production, but as oestrogen falls, we become insulin resistant. Progesterone becomes so important during menopause as it’s our calming hormone that also helps us to sleep properly through the night, but to make it we need glucose. As such, aim to cycle your carbs and have some higher carb days where you eat more root veg or squash during the month. Also consume more of these healthy complex carbs for recovery after exercising. If you’re peri-menopausal and still having a cycle, then ensure that you make the final week before your period higher in nature’s carbs as this is when your body is making the most progesterone.
- Get rid of bad fats and eat more of the good ones. Ditch the refined vegetable and seed oils (yellow oils) and get rid of trans fats by cutting out all processed foods. Ensure that the only fats you consume are healthy ones like extra virgin olive oil, extra virgin coconut oil, true nuts (e.g. walnuts, pecans, almonds, pistachios, hazelnuts – not cashews or peanuts that are legumes, not nuts), olives, coconut MCT oil (ideally a mix of C8 & C10) and avocados (fruit and oil). Fatty fish (salmon, mackerel, lake trout, herring, albacore tuna, anchovies, sardines) and their eggs (like caviar and salmon roe) are the best natural sources of DHA, an omega-3 essential fatty acid that our brains crave most. It’s key to have sufficient healthy fats in your diet so that your body can switch from burning sugars to fat-burning, where your body makes ketones. This is how you combat low brain energy during menopause – you switch from burning mainly sugars in the form of glucose, to ensuring you have a good supply of clean burning fuel in the form of ketones.
- Fall in love with fibre. Fibre stabilises blood sugar and insulin, digests more slowly, is more filling and is a food substate for gut microbes. We need both soluble (small leafy green, fruits, root veg, pumpkin, squash) and insoluble fibre (large green leaves, radishes, rocket, broccoli, brussel sprouts). Leave the skins on your sweet potatoes for more fibre. During peri- and menopause, we need more fibre, so aim for at least 30g a day.
- Include foods that provide phytoestrogens and lignans (which bind to receptor sites and can mimic the effects of oestrogen). Flax seeds, sesame seeds, chickpeas (that have been pressure-cooked first to remove the lectins), berries, melon, apples and apricots. Thankfully dark chocolate (85% or 90%) is very much your friend and also contains, antioxidants and some phytoestrogens, as well as theobromine (from cacao), which contributes a range of health benefits. The most well-studied phytoestrogens come from soy, but my suggestion would be to always follow the Japanese by only consuming fermented soy like natto, miso and tempeh. Unfermented soy can be extremely unfriendly for the gut.
- Eat a rainbow every day. Ensure you’re including the 6 colours of nature’s palette in your vegetable and fruit intake daily to maximise your supply of antioxidants. Our brain suffers the most from ‘oxidative stress’, a condition that occurs when the level of free radicals exceeds that which our body can counteract. The more free radicals your brain harbours, the more damage is done and protecting our neurons in menopause will see us through our brain-healthy senior years.
- Fasting needs to become your friend. Intermittent fasting is usually the best choice for our health through adulthood (except pregnancy) because it mimics our evolutionary norm in that we’ve been built for famine, not for feasting. During menopause, it becomes even more essential to maintain insulin sensitivity, burn belly fat and keep inflammation at bay. Fasting also triggers our inbuilt protection against chronic disease and keeps our brains sharp and fog-free. Cycle between intermittent fasting (16-18 hrs) and longer fasts of 36, 48 or 72 hours to enhance all the benefits, but especially burn belly fat. During your fast, in the absence of carbs (sugars) your body must burn fats—ketones—for energy, hence the term ‘ketogenic’. If you still have a menstrual cycle then only do the longer fasts in the first 10 days after your period when your oestrogen is high.
Ketones were, and still are, nature’s way of ensuring that communities would be able to benefit from the wisdom of older women. Ketones will prevent your brain from losing energy during menopause and also protect your neurons, but you need to first make the dietary changes outlined above and then adapt your body to fasting to make it happen. Look at any indigenous tribe and see how they revere the Grandmothers (who have almost no incidence of dementia or Alzheimer’s disease). We have a long way to go in the western world when it comes to respecting our elders, but the first important step to take is to protect your brain so that you can share your wisdom.
Okinawa is known as a Blue Zone given the number of people living to 100 and beyond. They credit their longevity to a practice called hara hachi bu that is all about stopping eating when they’re just 80% full, which is a great way to start your fasting journey.
NB: please don’t consider any longer fasts till you’ve conditioned your body and can do 18 or 20 hours with ease. You can find the steps to healthy fasting in our book, RESET EATING. My experience is that it takes most people 8-12 weeks to shift their metabolic set point sufficiently to go 18 hours without food. Take it slow and you won’t look back!
- Manage stress, prioritise sleep and maintain physical activity. Stress can steal your oestrogens. As cortisol increases your oestrogens go down, so anything you can do to reduce your stress load will not only help you, but better support your brain during menopause. Adequate quality sleep is essential for brain regeneration, which is supported by your nutrition choices, ensuring you’re eating as much for your progesterone level as you are for your oestrogens. The amount of physical activity you undertake maintains your muscle tissue, keeps you insulin sensitive, lowers stress levels and is a major component of remaining metabolically flexible and resilient.
- Hormone replacement therapy. It is possible to use hormone replacement therapy (HRT) to protect your brain as you transition through menopause. As we’ve outlined previously, my suggestion, if you choose this, would be to explore bioidentical hormone replacement therapy (BHRT / cBHT) with a doctor who specialises in it.
>>> If you’re not already signed up for the ANH International weekly newsletter, sign up for free now using the SUBSCRIBE button at the top of our website – or better still – become a Pathfinder member and join the ANH-Intl tribe to enjoy benefits unique to our members.
>> Feel free to republish – just follow our Alliance for Natural Health International Re-publishing Guidelines
>>> Return to ANH International homepage